by: Dr. Larry Sosna
Regrowth of neurons… also called Neuro-Regeneration is one of the most complicated
issues in the field of medical/science. The subject matter concerns the repair and
regrowth of nerve cells called neurons. The long body of the neuron is called the Axon.
This issue is divided into two imperative groups…. Peripheral Nervous System (PNS)
and the Central Nervous System (CNS) characterized by the brain and spinal cord.
When I took High School Biology the teacher made a clear and emphatic
statement. Central Nervous System neurons NEVER heal. He went on to state, that
Peripheral Neurons do heal but slowly. In Biology and Biochemistry at undergraduate
work in college both professors made the exact same statement my high school biology
teach made almost by rote. Never one to fully agree with such absolute matters in
science my questions were so penetrating and complex as to be unanswerable which
gained respect by one Professor and benign neglect from the second Professor
PNS has a method of regeneration to the injured neurons followed by the quick release
of white blood cells to fight infection. Schwann cells release neurotropic factors which
enhance regrowth of PNS neurons in several ways. The Schwann cells, prevent to
much cytotoxicity which is generally part of the healing process but illicit’s far to much
inflammation for regeneration to proceed normally. Schwann cells, also set up tubes
along side the damaged neuron. These tubes are even connected to the injured
degraded PNS neuron and a host of healing biochemicals are release by the tube to
stop neural degradation and provide healing repair to the affected injured neuron.
There are a host of outside interventions that can make this process go faster but I will
save them for Regeneration of the brain and spinal cord, which please remember is
still thought in many universities even taught to this day that CNS neurons cannot
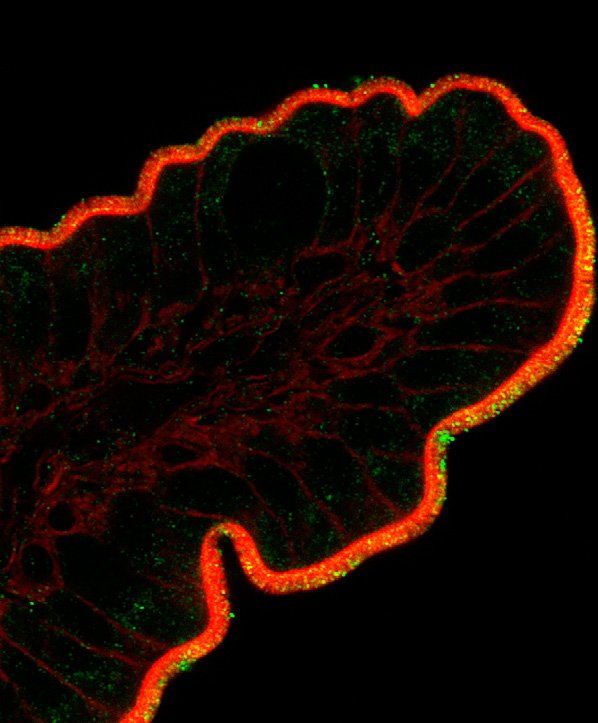
Regeneration and Repair of the Central Nervous System (Brain and Spinal Cord. There
are two types of cells meant to serve and protect CNS neurons from injury. They are
called Astrocytes and Gllial cells. It may be hard to believe but there are many more
astrocytes in the brain then there are brain Neurons and there are some 15 to 18 billion
brain neurons. Normally, after injury to brain neurons…astrocytes support neurons by
providing antioxidant protection.
The Good the Bad and the Ugly
While the Astrocytes bring in many antioxidants to prevent free radical oxidative toxic
damage to the brain neurons…they also over-react and allow for too much inflammation
and cytotoxins from white blood cell production of Interleukin-2 and 6… this is called up-
regulation of immune cell activity. It can destroy brain neurons faster then the initial
injury to a brain or spinal neurons. This process
brings about even more inflammation to try and carry away all of the dead cells,
including neurons and astrocytes as well as white blood cell waste deposits.
Unfortunately the brain is limited in size and to much inflammation causes intracranial
pressure to the point where brain infarct is possible without making a surgical opening in
the cranium to release the pressure….that is the bad and the ugly.
How do we solve the above dire situation and bring about brain cell neuron
In some cases like bacterial or viral Encephalitis of the brain and spinal cord
many neurons can be killed or injured due to massive white blood cell
proliferation. The white blood cells kill the bacteria and virus that causes
Encephalitis but the situation is so dramatic that in order for the brain to survive
the infection killing neurons…the message which signals the white blood cells to
enter the brain becomes so up-regulated that cannot down-regulate to a normal
response thus further killing both infected neurons and the infected brain cells
both. Many people die from this berserk super up-regulated immune response
stuck on full throttle. It is a vicious repetitive cycle.
We can stop this deathly cycle by giving the patient large intravenous doses of
Gamma Globulin. Gamma Globulin consists of every type of antibody the human
body can make. Scientists are not exactly certain how and why this has such a
profound normalizing effect immunologically but it does. It is called Immuno-
modulation to the normal set point.
In both Stroke patients and infection based Encephalitis of the brain… Immuno-
Modulation to a normal set point is a must in order for neuron cell death to stop and for
Certain biochemical factors play a vital role to decrease astrocytes! Cyclin Kinase
decreases astrocyte proliferation, increasing neuron function and recovery. Caffeic acid,
alpha- melanocyte stimulating hormone and cliostazol are all highly beneficial. They are
considered essential to a improved condition by reducing astrocyte production…this
treatment shows a decrease in neuron injury, the decrease in astrocyte high levels of
production is associated with a more positive and improved outcome moving toward
In 1984, I experienced a life/death illness called Herpetic Viral Encephalitis. It was
misdiagnosed my Manhattans most elite doctors…virtually always fatal, I lived and due
to the fact the death rate is so nearly complete I spent 3 years in bed and several more
in a wheel chair. There was no internet, no smart phones, just a nearly destroyed brain
with pain so blinding it felt as if two ice picks were being run through both eyes… and
trying to escape by pushing through the back of my skull. Luckily for me the feelers I
sent out daily… resulted in a call from Nobel prize winning doctor and scientist, Dr. Rita
Levi Montalcini who won the Nobel Prize for the discovery of Embryonic Fetal Nerve
Growth Factor in 1986. I was the first human to ever get shots of Fetal Nerve Growth
Factor in 1988 to grow back and regenerate my damaged brain neurons. Then this
magnificent woman became my mentor….I still live speaking to her shadow everyday as
she passed over at the age of almost 104.
Rita Levi-Montalcini’s discovery of a protein called ‘fetal nerve growth factor,”
which fosters the growth of nerve fibers and also plays a role in the brain and the immune
system, is one of the most important steps taken so far toward understanding how the
fantastically complex system of nerves is laid down and linked to the tissues in a developing
embryo. Her account of the adventures leading to this discovery, for which she won a Nobel
Prize in Physiology and Medicine in 1986, has a special contemporary interest. We now
know her discovery is how the brain grows all of it’s neurons when one is an embryo inside
one’s mothers womb until birth and sustains, protects and regenerates brain neurons if one
is fortunate to be born with a large amount of FNGF . Thank goodness she was able to scale
it up through a deal with a large cutting edge biotechnology lab. in Montreal. They are the
ONLY Lab. in the world to this day that makes Dr. Rita’s original formulations.
We at AA,I are indeed incredibly fortunate to be able to have access to her formulations at
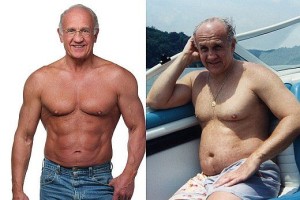
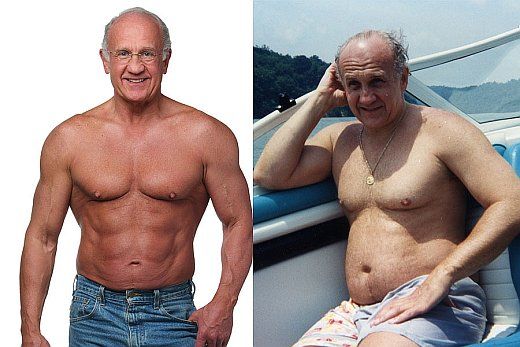
I combined her fetal nerve growth factors with very youthful blood levels of HGH (human
growth hormone…levels that would be normal for the average healthy 16 year old. Eighteen
months later, I was completely better in every way… brain regeneration wise… and in every
other health manner. The addition of HGH was my inspiration as it has been known for
many decades that it is HGH which mobilizes all of the fetal tissue growth factors such as
cardiac tissue growth factor…to do protein synthesis and thus regeneration of the heart
AND all other tissues contained within the human body. Without youthful blood levels of
HGH(say blood levels normal for a healthy 26 year old to 30 year old) and credible levels of
fetal nerve growth factor… regrowth of Neurons is unlikely in the extreme BUT with these
safe and effective blood levels of both Regrowth of every type of Neuron is probable in and
that brings amazing hope. The only Regrowth we cannot master yet is CNS spinal cord cut
in half…but the army medical scientists are getting very close.
Imagine how old we would all look, if we did not have adequate cell levels of
epithelial (skin tissue growth factor) to regenerate our SKIN? So, just like
hormones, as we age we lose our tissue growth factors…and if they cannot be
replaced to the optimal level from exogenous sources we will all be subject to
the ravages of age related illness.
Gratefully, here at AAI we have all critical tissue growth factors available to
you, our beloved family of clients.
Kindly, Larry Sosna PhD HHP
1. Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB,
Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V,
Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian
D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Thom T,
Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics–2010
update: a report from the American Heart
Association.Circulation. 2010;121:e46–e215. [PubMed]
2. Blakeley JO, Llinas RH. Thrombolytic therapy for acute ischemic stroke. J. Neurol.
Sci. 2007;261:55–62.[PubMed]
3. Marder VJ, Jahan R, Gruber T, Goyal A, Arora V. Thrombolysis with plasmin: implications
for stroke treatment. Stroke. 2010;41:S45–S49. [PMC free article] [PubMed]
4. Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment
of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N. Engl. J.
Med.2002;346:557–563. [PubMed]
5. Howells DW, Porritt MJ, Rewell SS, O’Collins V, Sena ES, van der Worp HB, Traystman RJ,
Macleod MR. Different strokes for different folks: the rich diversity of animal models of focal
cerebral ischemia. J. Cereb. Blood Flow Metab. 30:1412–1431. [PMC free article] [PubMed]
6. Kettenmann H, Ramson BR. Neuroglia. New York: Oxford University Press; 1995.
7. Nedergaard M, Ransom B, Goldman SA. New roles for astrocytes: redefining the functional
architecture of the brain. Trends Neurosci. 2003;26:523–530. [PubMed]
8. Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta
Neuropathol. 2010;119:7–35.[PMC free article] [PubMed]
9. Goldberg MP, Choi DW. Combined oxygen and glucose deprivation in cortical cell culture:
calcium-dependent and calcium-independent mechanisms of neuronal injury. J.
Neurosci. 1993;13:3510–3524.[PubMed]
10. Swanson RA, Ying W, Kauppinen TM. Astrocyte influences on ischemic neuronal
death. Curr. Mol. Med. 2004;4:193–205. [PubMed]
11. Dringen R, Hirrlinger J. Glutathione pathways in the brain. Biol.
Chem. 2003;384:505–516. [PubMed]
12. Wilson JX. Antioxidant defense of the brain: a role for astrocytes. Can. J. Physiol.
Pharmacol.1997;75:1149–1163. [PubMed]
13. Rossi DJ, Brady JD, Mohr C. Astrocyte metabolism and signaling during brain
ischemia. Nat. Neurosci.2007;10:1377–1386. [PubMed]
14. Nedergaard M, Dirnagl U. Role of glial cells in cerebral
ischemia. Glia. 2005;50:281–286. [PubMed]
15. Ouyang YB, Voloboueva LA, Xu LJ, Giffard RG. Selective dysfunction of hippocampal
CA1 astrocytes contributes to delayed neuronal damage after transient forebrain ischemia. J.
Neurosci.2007;27:4253–4260. [PMC free article] [PubMed]
16. Xu L, Emery JF, Ouyang YB, Voloboueva LA, Giffard RG. Astrocyte targeted
overexpression of Hsp72 or SOD2 reduces neuronal vulnerability to forebrain
ischemia. Glia. 2010;58:1042–1049.[PMC free article] [PubMed]
17. Anderson MF, Blomstrand F, Blomstrand C, Eriksson PS, Nilsson M. Astrocytes and stroke:
networking for survival? Neurochem. Res. 2003;28:293–305. [PubMed]
18. Giffard RG, Swanson RA. Ischemia-induced programmed cell death in
astrocytes. Glia. 2005;50:299–306. [PubMed]
19. Almeida A, Delgado-Esteban M, Bolanos JP, Medina JM. Oxygen and glucose deprivation
induces mitochondrial dysfunction and oxidative stress in neurones but not in astrocytes in
primary culture. J. Neurochem. 2002;81:207–217. [PubMed]
20. Xu L, Sapolsky RM, Giffard RG. Differential sensitivity of murine astrocytes and neurons
from different brain regions to injury. Exp. Neurol. 2001;169:416–424. [PubMed]
21. Zhao G, Flavin MP. Differential sensitivity of rat hippocampal and cortical astrocytes to
oxygen-glucose deprivation injury. Neurosci. Lett. 2000;285:177–180. [PubMed]
22. Lukaszevicz AC, Sampaio N, Guegan C, Benchoua A, Couriaud C, Chevalier E, Sola B,
Lacombe P, Onteniente B. High sensitivity of protoplasmic cortical astroglia to focal ischemia. J.
Cereb. Blood Flow Metab. 2002;22:289–298. [PubMed]
23. Bondarenko A, Chesler M. Rapid astrocyte death induced by transient hypoxia, acidosis, and
extracellular ion shifts. Glia. 2001;34:134–142. [PubMed]
24. Giffard RG, Monyer H, Choi DW. Selective vulnerability of cultured cortical glia to injury
by extracellular acidosis. Brain Res. 1990;530:138–141. [PubMed]
25. Swanson RA, Farrell K, Stein BA. Astrocyte energetics, function, and death under conditions
of incomplete ischemia: a mechanism of glial death in the
penumbra. Glia. 1997;21:142–153. [PubMed]
26. Tombaugh GC, Sapolsky RM. Mechanistic distinctions between excitotoxic and acidotic
hippocampal damage in an in vitro model of ischemia. J. Cereb. Blood Flow
Metab. 1990;10:527–535. [PubMed]
27. Chen Y, Swanson RA. Astrocytes and brain injury. J. Cereb. Blood Flow
Metab. 2003;23:137–149.[PubMed]
28. Lee MH, Kim H, Kim SS, Lee TH, Lim BV, Chang HK, Jang MH, Shin MC, Shin MS, Kim
CJ. Treadmill exercise suppresses ischemia-induced increment in apoptosis and cell proliferation
in hippocampal dentate gyrus of gerbils. Life Sci. 2003;73:2455–2465. [PubMed]
29. Li Y, Chopp M, Zhang ZG, Zhang RL. Expression of glial fibrillary acidic protein in areas of
focal cerebral ischemia accompanies neuronal expression of 72-kDa heat shock protein. J.
Neurol. Sci.1995;128:134–142. [PubMed]
30. Schroeter M, Schiene K, Kraemer M, Hagemann G, Weigel H, Eysel UT, Witte OW, Stoll G.
Astroglial responses in photochemically induced focal ischemia of the rat cortex. Exp Brain
Res. 1995;106:1–6.[PubMed]
31. Van Beek J, Chan P, Bernaudin M, Petit E, MacKenzie ET, Fontaine M. Glial responses,
clusterin, and complement in permanent focal cerebral ischemia in the
mouse. Glia. 2000;31:39–50. [PubMed]
32. Yamashita K, Vogel P, Fritze K, Back T, Hossmann KA, Wiessner C. Monitoring the
temporal and spatial activation pattern of astrocytes in focal cerebral ischemia using in situ
hybridization to GFAP mRNA: comparison with sgp-2 and hsp70 mRNA and the effect of
glutamate receptor antagonists. Brain Res.1996;735:285–297. [PubMed]
33. Liu D, Smith CL, Barone FC, Ellison JA, Lysko PG, Li K, Simpson IA. Astrocytic demise
precedes delayed neuronal death in focal ischemic rat brain. Brain Res. Mol. Brain
Res. 1999;68:29–41. [PubMed]
34. Dugan LL, Bruno VM, Amagasu SM, Giffard RG. Glia modulate the response of murine
cortical neurons to excitotoxicity: glia exacerbate AMPA neurotoxicity. J.
Neurosci. 1995;15:4545–4555. [PubMed]
35. Rosenberg PA, Aizenman E. Hundred-fold increase in neuronal vulnerability to glutamate
toxicity in astrocyte-poor cultures of rat cerebral cortex. Neurosci.
Lett. 1989;103:162–168. [PubMed]
36. Voloboueva LA, Suh SW, Swanson RA, Giffard RG. Inhibition of mitochondrial function in
astrocytes: implications for neuroprotection. J. Neurochem. 2007;102:1383–1394. [PMC free
37. Chen JC, Hsu-Chou H, Lu JL, Chiang YC, Huang HM, Wang HL, Wu T, Liao JJ, Yeh TS.
Down-regulation of the glial glutamate transporter GLT-1 in rat hippocampus and striatum and
its modulation by a group III metabotropic glutamate receptor antagonist following transient
global forebrain ischemia. Neuro-pharmacology. 2005;49:703–714. [PubMed]
38. Yeh TH, Hwang HM, Chen JJ, Wu T, Li AH, Wang HL. Glutamate transporter function of
rat hippocampal astrocytes is impaired following the global ischemia. Neurobiol.
Dis. 2005;18:476–483.[PubMed]
39. Ito U, Hakamata Y, Kawakami E, Oyanagi K. Degeneration of astrocytic processes and their
mitochondria in cerebral cortical regions peripheral to the cortical infarction: heterogeneity of
their disintegration is closely associated with disseminated selective neuronal necrosis and
maturation of injury.Stroke. 2009;40:2173–2181. [PubMed]
40. Ito U, Hakamata Y, Kawakami E, Oyanagi K. Temporary focal cerebral ischemia results in
swollen astrocytic end-feet that compress microvessels and lead to focal cortical infarction. J.
Cereb. Blood Flow Metab. 2010 [PMC free article] [PubMed]
41. Vangeison G, Rempe DA. The Janus-faced effects of hypoxia on astrocyte
function. Neuroscientist.2009;15:579–588. [PMC free article] [PubMed]
42. Bidmon HJ, Jancsik V, Schleicher A, Hagemann G, Witte OW, Woodhams P, Zilles K.
Structural alterations and changes in cytoskeletal proteins and proteoglycans after focal cortical
ischemia. Neuroscience.1998;82:397–420. [PubMed]
43. Yasuda Y, Tateishi N, Shimoda T, Satoh S, Ogitani E, Fu-jita S. Relationship between
S100beta and GFAP expression in astrocytes during infarction and glial scar formation after mild
transient ischemia. Brain Res. 2004;1021:20–31. [PubMed]
44. Smith GM, Strunz C. Growth factor and cytokine regulation of chondroitin sulfate
proteoglycans by astrocytes. Glia. 2005;52:209–218. [PubMed]
45. Gris P, Tighe A, Levin D, Sharma R, Brown A. Transcriptional regulation of scar gene
expression in primary astrocytes. Glia. 2007;55:1145–1155. [PubMed]
46. Martinez AD, Saez JC. Regulation of astrocyte gap junctions by hypoxia-
reoxygenation. Brain Res. Brain Res. Rev. 2000;32:250–258. [PubMed]
47. Lin JH, Weigel H, Cotrina ML, Liu S, Bueno E, Hansen AJ, Hansen TW, Goldman S,
Nedergaard M. Gap-junction-mediated propagation and amplification of cell injury. Nat.
Neurosci. 1998;1:494–500.[PubMed]
48. Wang W, Redecker C, Yu ZY, Xie MJ, Tian DS, Zhang L, Bu BT, Witte OW. Rat focal
cerebral ischemia induced astrocyte proliferation and delayed neuronal death are attenuated by
cyclin-dependent kinase inhibition. J. Clin. Neurosci. 2008;15:278–285. [PubMed]
49. Forslin Aronsson S, Spulber S, Popescu LM, Winblad B, Post C, Oprica M, Schultzberg M.
alpha-Melanocyte-stimulating hormone is neuroprotective in rat global cerebral
ischemia. Neuropeptides.2006;40:65–75. [PubMed]
50. Fang SH, Wei EQ, Zhou Y, Wang ML, Zhang WP, Yu GL, Chu LS, Chen Z. Increased
expression of cysteinyl leukotriene receptor-1 in the brain mediates neuronal damage and
astrogliosis after focal cerebral ischemia in rats. Neuroscience. 2006;140:969–979. [PubMed]
51. Ye YL, Shi WZ, Zhang WP, Wang ML, Zhou Y, Fang SH, Liu LY, Zhang Q, Yu YP, Wei
EQ. Cilostazol, a phosphodiesterase 3 inhibitor, protects mice against acute and late ischemic
brain injuries. Eur. J. Pharmacol. 2007;557:23–31. [PubMed]
52. Zhou Y, Fang SH, Ye YL, Chu LS, Zhang WP, Wang ML, Wei EQ. Caffeic acid ameliorates
early and delayed brain injuries after focal cerebral ischemia in rats. Acta Pharmacol.
Sin. 2006;27:1103–1110.[PubMed]
53. Chung JH, Lee EY, Jang MH, Kim CJ, Kim J, Ha E, Park HK, Choi S, Lee H, Park SH,
Leem KH, Kim EH. Acupuncture decreases ischemia-induced apoptosis and cell proliferation in
dentate gyrus of gerbils. Neurol. Res. 2007;29 Suppl 1:S23–S27. [PubMed]
54. del Zoppo GJ. Inflammation and the neurovascular unit in the setting of focal cerebral
ischemia.Neuroscience. 2009;158:972–982. [PMC free article] [PubMed]
55. Kaur C, Ling EA. Blood brain barrier in hypoxic-ischemic conditions. Curr. Neurovasc.
Res. 2008;5:71–81. [PubMed]
56. Nawashiro H, Brenner M, Fukui S, Shima K, Hallenbeck JM. High susceptibility to cerebral
ischemia in GFAP-null mice. J. Cereb. Blood Flow Metab. 2000;20:1040–1044. [PubMed]
57. Li L, Lundkvist A, Andersson D, Wilhelmsson U, Nagai N, Pardo AC, Nodin C, Stahlberg
A, Aprico K, Larsson K, Yabe T, Moons L, Fotheringham A, Davies I, Carmeliet P, Schwartz
JP, Pekna M, Kubista M, Blomstrand F, Mara-gakis N, Nilsson M, Pekny M. Protective role of
reactive astrocytes in brain ischemia. J. Cereb. Blood Flow Metab. 2008;28:468–481. [PubMed]
58. Kinoshita A, Yamada K, Kohmura E, Hayakawa T. Effect of astrocyte-derived factors on
ischemic brain edema induced by rat MCA occlusion. APMIS. 1990;98:851–857. [PubMed]
59. Buchhold B, Mogoanta L, Suofu Y, Hamm A, Walker L, Kessler C, Popa-Wagner A.
Environmental enrichment improves functional and neuropathological indices following stroke
in young and aged rats.Restor. Neurol. Neurosci. 2007;25:467–484. [PubMed]
60. Keiner S, Wurm F, Kunze A, Witte OW, Redecker C. Rehabilitative therapies differentially
alter proliferation and survival of glial cell populations in the perilesional zone of cortical
infarcts. Glia.2008;56:516–527. [PubMed]
61. Popa-Wagner A, Badan I, Walker L, Groppa S, Patrana N, Kessler C. Accelerated infarct
development, cytogenesis and apoptosis following transient cerebral ischemia in aged rats. Acta
Neuropathol.2007;113:277–293. [PubMed]
62. Li Y, Chen J, Zhang CL, Wang L, Lu D, Katakowski M, Gao Q, Shen LH, Zhang J, Lu M,